Psoriasis Worsened by Drugs: What Medications Trigger Flares and How to Avoid Them
When psoriasis worsened by drugs, a condition where certain medications cause skin plaques to flare or become more severe. Also known as drug-induced psoriasis, it’s not rare—and it’s often missed because the link isn’t obvious. You might be taking a pill for high blood pressure, depression, or arthritis, and not realize it’s making your skin worse. This isn’t just about irritation—it’s about your immune system reacting in ways that turn mild psoriasis into a painful, visible flare.
Some of the most common culprits include beta-blockers, medications used to treat high blood pressure and heart conditions, which can slow down skin cell turnover in a way that traps dead cells under the surface, triggering plaques. Lithium, a mood stabilizer used for bipolar disorder, is another big one—it interferes with immune signaling and can make psoriasis up to 50% worse in some people. Even antimalarials, drugs like hydroxychloroquine used for lupus or malaria prevention, have been tied to sudden, severe outbreaks. And if you’re on NSAIDs for joint pain, you might think they’re helping your psoriatic arthritis—until they don’t. In some cases, they make both the skin and joints flare together.
The good news? Not everyone reacts the same way. Your body’s response depends on genetics, how long you’ve had psoriasis, and what other conditions you’re managing. That’s why it’s not about avoiding all these drugs—it’s about knowing the risks and talking to your doctor before starting or switching anything. If your skin suddenly flares after starting a new medication, don’t assume it’s stress or diet. Track it. Write down when the flare started and what changed. Bring that to your provider. Sometimes, switching to a different class of drug—like swapping a beta-blocker for an ACE inhibitor—can make all the difference without losing the health benefit you need.
And it’s not just about the drugs you take directly. Some treatments for other autoimmune conditions, like TNF inhibitors used for rheumatoid arthritis, can paradoxically trigger psoriasis in people who didn’t have it before. That’s why understanding the link between psoriatic arthritis, an autoimmune disease that affects both skin and joints and medication use matters. If you have joint pain and scaly skin, you might be dealing with both—and the wrong drug could make both worse.
Below, you’ll find real-world insights from people who’ve been there: which drugs caused their flares, what alternatives worked, and how they learned to spot the warning signs before it got out of hand. These aren’t theory pieces—they’re lived experiences backed by clinical patterns. Whether you’re managing psoriasis yourself or helping someone who is, this collection gives you the practical, no-fluff facts you need to ask the right questions and protect your skin.
Psoriasis and Beta-Blockers: What You Need to Know About Skin Flare Risk
By Lindsey Smith On 7 Dec, 2025 Comments (15)
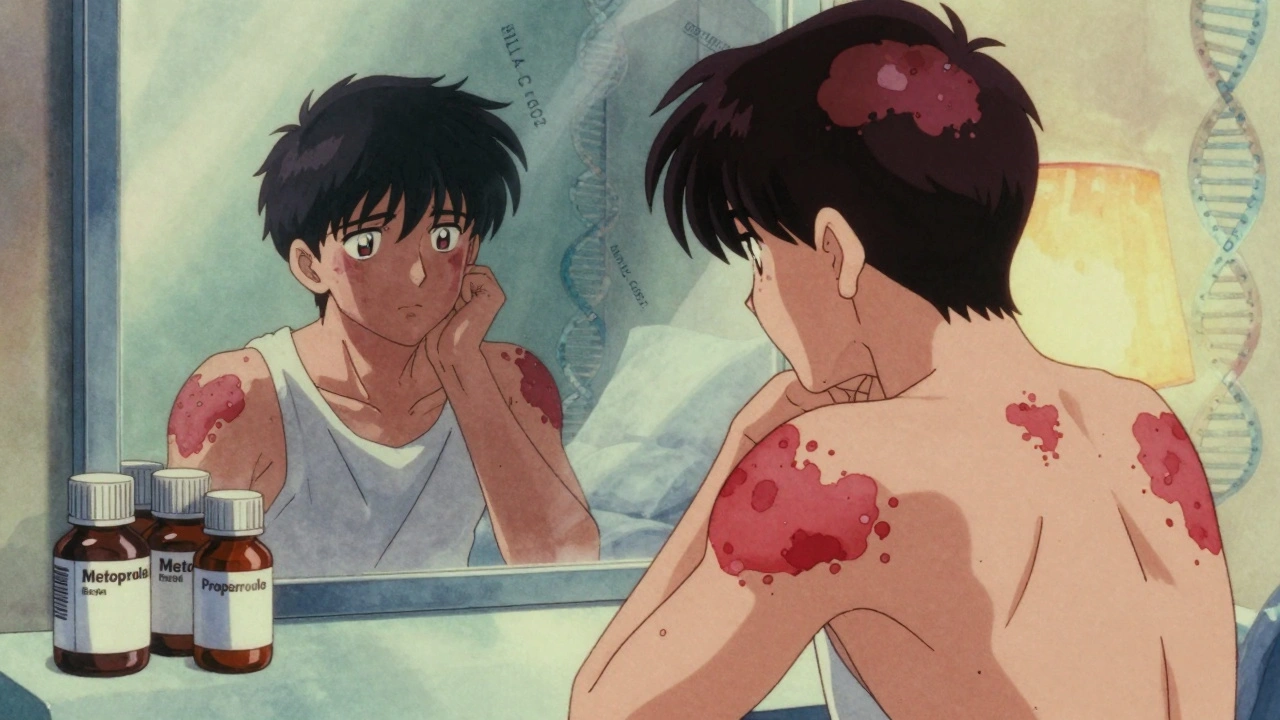
Beta-blockers can trigger or worsen psoriasis in up to 20% of users, with flares appearing months after starting the drug. Learn which medications carry the highest risk and what to do if your skin reacts.
View More