CHA2DS2-VASc Stroke Risk Calculator
Calculate Your Stroke Risk
This tool helps you understand your stroke risk from atrial fibrillation compared to fall-related bleeding risk. It's designed to help you and your doctor make informed decisions about anticoagulation therapy.
Results
Your CHA2DS2-VASc Score:
Estimated Annual Stroke Risk:
Annual Fall-Related Bleeding Risk (DOACs):
According to clinical guidelines, patients with a score of 2 or higher (men) or 3 or higher (women) should receive anticoagulation therapy. Your score indicates .
Important: The risk of stroke (3-5% per year for your score) is significantly higher than the risk of serious brain bleeding from falls (0.2-0.5% per year) while on DOACs. Stopping anticoagulants due to fall risk alone can increase your stroke risk by 300-400%.
Many older adults on blood thinners are told to stop their medication because they’re at risk of falling. But here’s the truth: fall risk alone should never be the reason to stop anticoagulants. In fact, stopping them because of falls often puts patients at greater risk - not from bleeding, but from stroke.
Why Falling Doesn’t Mean Stopping Blood Thinners
It’s a common fear: if you’re on a blood thinner and you fall, you might bleed badly. That sounds scary, and it’s why some doctors avoid prescribing anticoagulants to older patients, especially those in nursing homes where falls are frequent. But data tells a different story.
For someone with atrial fibrillation (AFib) and a CHA2DS2-VASc score of 3 or higher, their annual stroke risk is between 3% and 5%. That’s 3 to 5 strokes per 100 people every year. Meanwhile, the risk of a serious brain bleed from a fall while on anticoagulants? Only about 0.2% to 0.5% per year. That’s less than one in 200 people.
Think about it this way: you’d have to fall nearly 300 times in a single year for the risk of bleeding to outweigh the benefit of preventing a stroke. That’s not just unlikely - it’s nearly impossible. And yet, many patients still get denied anticoagulation because they’ve had one or two falls.
What Anticoagulants Are Safe for Fallers?
Not all blood thinners are the same. Warfarin has been around for decades, but it’s messy to manage. It requires regular blood tests, interacts with food and other meds, and carries a higher risk of brain bleeds.
Direct Oral Anticoagulants (DOACs) - like apixaban, rivaroxaban, dabigatran, and edoxaban - are now the first choice for most patients. Why? Because they reduce the risk of intracranial hemorrhage by 30% to 50% compared to warfarin. They don’t need routine blood tests. They have fewer interactions. And for someone who’s prone to falls, that’s a game-changer.
According to 2022 data from IQVIA, DOACs now make up about 80% of new prescriptions for AFib in the U.S. That’s not because they’re trendy - it’s because they’re safer for older, fall-prone patients.
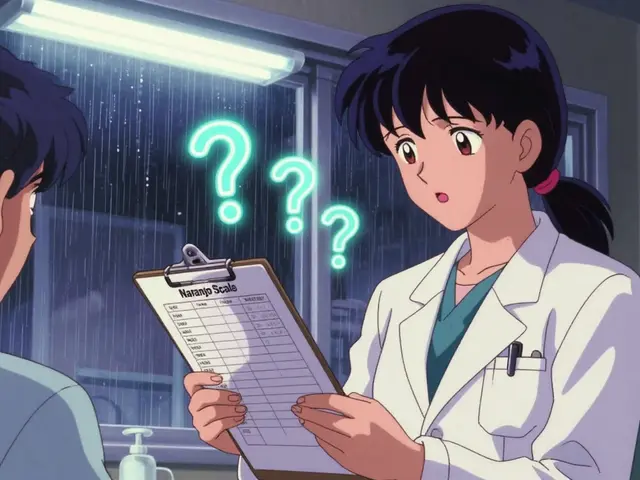
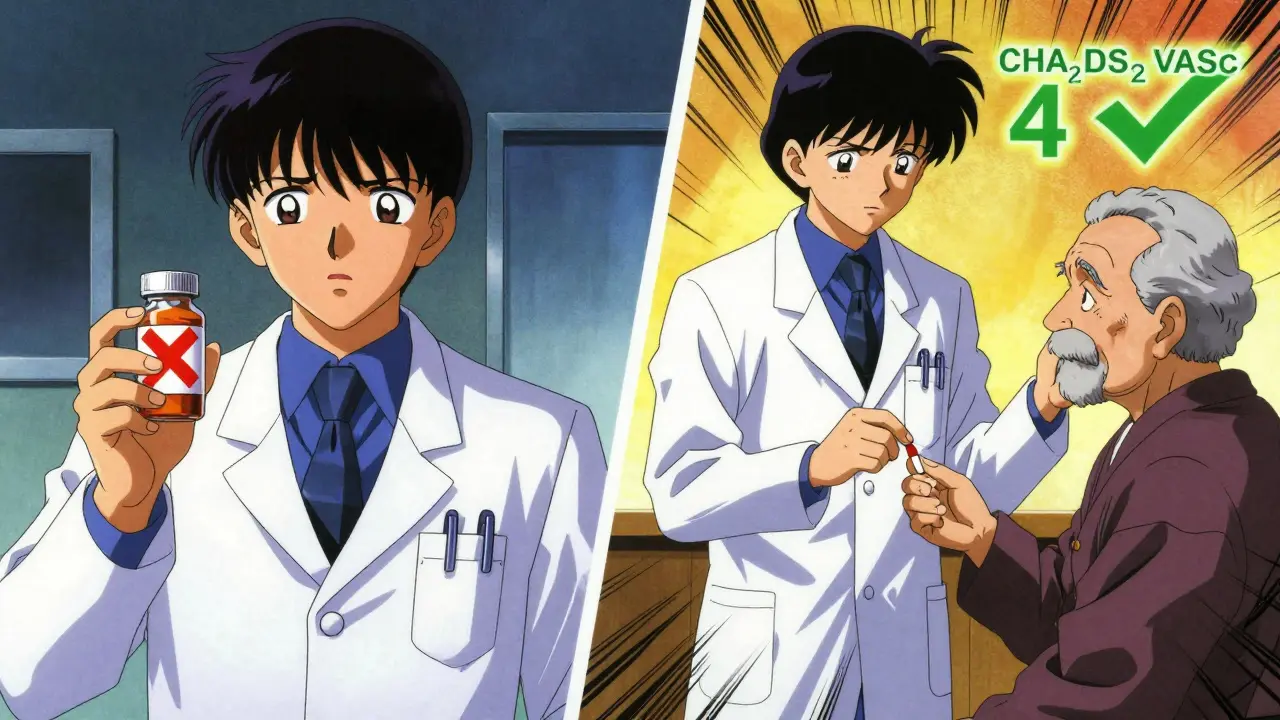
How to Know If You Need Anticoagulation
Not everyone with AFib needs a blood thinner. But if you’re over 65, have high blood pressure, diabetes, heart failure, or a history of stroke, your risk goes up. That’s where the CHA2DS2-VASc score comes in.
- Score of 2 or higher in men? Anticoagulation recommended.
- Score of 3 or higher in women? Anticoagulation recommended.
That’s it. Fall risk doesn’t change that. A 78-year-old who fell last month but has a CHA2DS2-VASc score of 4 still has a 4% chance of having a stroke this year. That’s four times higher than their chance of a serious brain bleed from a fall while on a DOAC.
There’s also the HAS-BLED score, which looks at bleeding risk factors like uncontrolled high blood pressure, kidney or liver problems, past bleeding, or heavy alcohol use. A score of 3 or higher means you need closer monitoring - not avoidance.
What You Should Do Instead of Stopping Medication
If you’re at risk of falling, the answer isn’t to stop your blood thinner. It’s to reduce the chances of falling in the first place.
Here’s what works:
- Review all your medications. Sedatives, sleeping pills, blood pressure drugs, and antidepressants can make you dizzy or unsteady. Some might be unnecessary. A pharmacist or geriatrician can help cut what’s not needed.
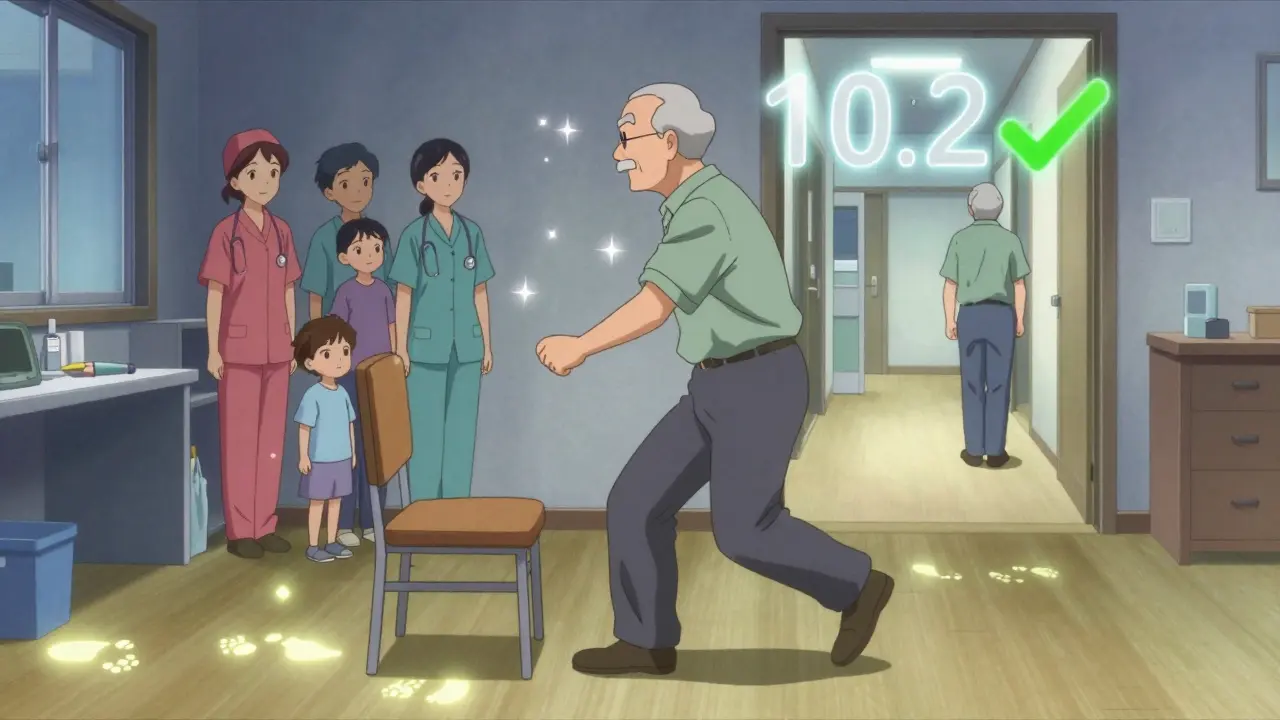
- Test your balance. The Timed Up and Go test is simple: sit in a chair, stand up, walk 10 feet, turn, walk back, and sit down. If it takes more than 12 seconds, your fall risk is high. Physical therapy can help.
- Check your vision. Cataracts, glaucoma, or outdated glasses? Get them fixed. Poor vision is one of the biggest causes of falls.
- Make your home safer. Remove throw rugs, install grab bars in the bathroom, add nightlights, and clear clutter. Even small changes cut falls by 30%.
- Manage low blood pressure when standing. If you feel lightheaded when getting up, talk to your doctor. This is called orthostatic hypotension - and it’s treatable.
These steps take time - maybe 30 to 60 minutes for a full assessment - but they’re worth it. Studies show that when you fix the environment and the meds, falls drop by 40% or more. And you stay protected from stroke.
What Not to Do
Some providers try to "lower the risk" by reducing the dose of a DOAC or aiming for a lower INR with warfarin. That’s dangerous.
DOACs don’t work like warfarin. Lowering the dose doesn’t make them safer - it makes them less effective. You’re trading stroke prevention for no real drop in bleeding risk. Same with warfarin: targeting an INR below 2.0 doesn’t prevent bleeds - it lets clots form.
Professional guidelines from the American College of Cardiology, the American Heart Association, and the European Society of Geriatric Medicine all say: don’t do this. It’s not just ineffective - it’s harmful.
When Might You Actually Skip Anticoagulation?
There are exceptions. If you have active bleeding, a severe bleeding disorder, or uncontrolled high blood pressure (systolic over 180), anticoagulation is unsafe. But those are medical emergencies - not everyday fall risks.
For very frail patients with life expectancy under a year, the math changes. Stroke prevention takes months to years to show benefit. If someone is unlikely to live that long, the benefit may not outweigh the risks. But that’s not about falling - it’s about overall health and goals of care.
That’s why shared decision-making matters. Talk to your doctor. Ask: "What’s my stroke risk? What’s my bleeding risk? What can we do to prevent falls?" Don’t accept "you fall too much" as an answer.
Why This Misconception Still Exists
Despite all the evidence, a 2023 review found that 40% to 50% of primary care doctors still believe fall risk alone should stop anticoagulation. Why? Because it’s easier. It feels safer to stop a drug than to fix a home or adjust meds.
But the real danger isn’t falling - it’s under-treating stroke risk. Hospitals are now being penalized by Medicare for not prescribing anticoagulants to eligible AFib patients. That’s because we know: untreated stroke causes more death and disability than falls ever do.
Patients who stop their blood thinners out of fear often end up in the hospital - not from a bleed, but from a stroke. And those strokes are usually worse because they weren’t prevented.
The Bottom Line
Fall risk doesn’t cancel out stroke risk. It just means you need a better plan - not no plan.
Keep your anticoagulant. Switch to a DOAC if you’re still on warfarin. Work with your care team to fix what you can control: your meds, your balance, your home, your vision. You don’t have to live in fear of falling. You just have to live smarter.
Should I stop my blood thinner if I’ve had a fall?
No. Having one or even a few falls doesn’t mean you should stop anticoagulation. The risk of stroke from untreated atrial fibrillation is far greater than the risk of a serious bleed from a fall. Instead of stopping your medication, focus on reducing fall risk through medication review, balance training, and home safety changes.
Are DOACs safer than warfarin for people who fall?
Yes. DOACs (like apixaban and rivaroxaban) reduce the risk of brain bleeding by 30% to 50% compared to warfarin. They also don’t require frequent blood tests or dietary restrictions. For older adults at risk of falls, DOACs are the preferred choice unless kidney function is severely impaired.
Can I lower my DOAC dose to make it safer?
No. Reducing the dose of a DOAC doesn’t lower bleeding risk - it increases stroke risk. DOACs are designed to work at specific doses. Skipping or lowering them without medical supervision can leave you unprotected from clots. Always follow the prescribed dose.
What’s the best way to prevent falls while on blood thinners?
Start with a multifactorial assessment: review medications (especially sedatives and blood pressure drugs), test balance with the Timed Up and Go test, check vision, remove home hazards like rugs and poor lighting, and treat dizziness when standing. Physical therapy and home safety modifications can reduce falls by 40% or more.
Is it okay to avoid anticoagulation just because I’m old?
No. Age alone is not a reason to avoid anticoagulation. In fact, older adults benefit the most from stroke prevention because their risk of AFib-related stroke increases with age. What matters is your CHA2DS2-VASc score, not your age. A 90-year-old with a score of 4 has the same stroke risk as a 70-year-old with the same score - and both need anticoagulation unless other factors make it unsafe.