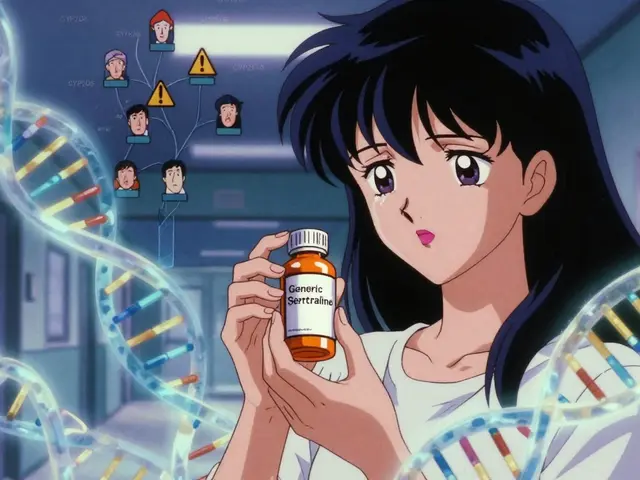
Every year, millions of people in the U.S. rely on generic drugs to manage chronic conditions like high blood pressure, diabetes, and depression. These medications are cheaper, often costing 80% less than brand-name versions. But behind the low price tag is a complex global supply chain where contamination can slip through - and the consequences aren’t just theoretical. In 2022, generic drug contamination was behind 37% of all drug recalls in the U.S., according to the FDA. That’s not a glitch. It’s a systemic risk.
How Contamination Happens in Generic Drugs
Contamination doesn’t mean dirt or dust. It’s when unwanted chemicals, microbes, or even leftover drug residues end up in a pill, capsule, or injection. This can happen at any stage: during the production of the active ingredient, mixing with other drugs on the same line, or even when a technician opens a vial. The most common types are chemical cross-contamination and microbial growth.One major source is shared manufacturing equipment. If a factory produces multiple drugs - say, an antihypertensive and an antidepressant - and doesn’t clean thoroughly between batches, tiny traces of one can end up in the other. The FDA requires that residue from previous products be reduced to 10 parts per million (ppm). But for highly potent drugs, like cancer treatments or hormones, even that amount can be dangerous. Experts like Dr. Michael Kopcha point out that this limit isn’t always science-based; it’s often a placeholder until companies do proper toxicology studies.
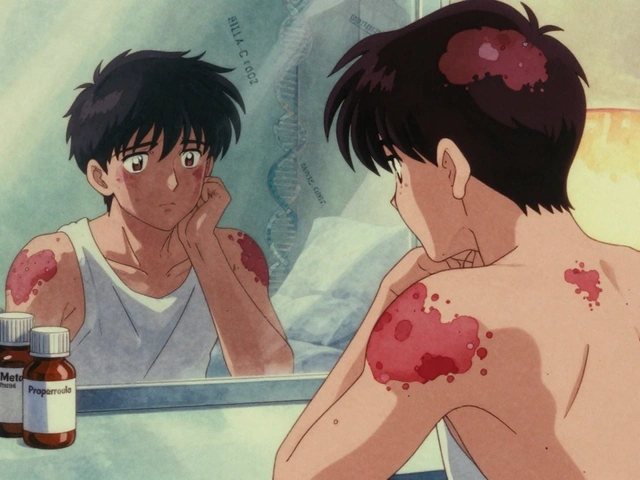
Microbial contamination is another big issue. Oral tablets can’t have more than 1,000 colony-forming units (CFU) of bacteria per gram, and mold must be under 100 CFU. Yet in 2021, a patient in Ohio developed severe skin burns from a generic hydrocortisone cream that tested positive for mold. The FDA’s MedWatch database recorded over 1,200 contamination reports between 2020 and 2022, with nearly 400 linked to actual harm.
Why Generic Drugs Are More at Risk
You might assume brand-name drugs are safer. They’re not. Both must meet the same FDA standards. But here’s the catch: generics are made under tighter financial pressure. While brand-name companies often have profit margins of 60-70%, generics operate at 20-25%. That leaves less room for investment in modern equipment, rigorous cleaning, or advanced testing.FDA inspection data from 2022 shows generic facilities had 8.3% of their inspections flagged for contamination control failures - compared to just 5.1% for brand-name makers. The problem is worse overseas. In India, where 60% of U.S. generic drugs are made, 12.7% of inspections found contamination issues. In contrast, U.S.-based facilities had only 6.4%. That’s not because Indian manufacturers are negligent - many are highly skilled - but because older factories, weaker oversight, and pressure to cut costs create blind spots.
Take the 2018-2019 valsartan recall. Nitrosamine impurities - carcinogenic chemicals - showed up in blood pressure meds from 22 manufacturers across eight countries. The problem? A single chemical change in the synthesis process, unnoticed for years. The fallout: over 2,300 recalls and $1.2 billion in losses. It wasn’t one bad plant. It was a global blind spot.
Human Error and Facility Design
It’s not just machines. People are the biggest source of contamination. In cleanrooms, a single person sheds 40,000 skin cells per minute and releases 100,000 particles larger than 0.3 microns just by standing still. That’s why gowning procedures, air showers, and strict movement rules exist. But in many facilities, training is rushed or skipped.Here’s what actually causes contamination in practice:
- Piercing a vial septum with a needle (62% of incidents)
- Withdrawing the needle from the vial (41%)
- Breaking glass ampules (28%)
These aren’t lab accidents. They’re routine steps in pharmacies and hospitals. OSHA found that 63% of compounding pharmacies lack proper engineering controls - like ventilated hoods - to protect workers and patients. In one case, pharmacists were handling cyclophosphamide, a chemotherapy drug, and found traces of it on 85% of their work surfaces. That’s not just a risk to patients. It’s a risk to the people giving the medicine.

What’s Being Done to Prevent It
Some companies are fixing the problem - and proving it’s possible. Teva Pharmaceuticals’ facility in Bologna, Italy, cut cross-contamination by 78% between 2018 and 2022. How? They switched to closed manufacturing systems. Instead of open mixers and exposed transfer lines, everything happens in sealed, automated units. No air exposure. No human touch. No chance for contamination.Other leaders are using real-time monitoring. Mylan’s Morgantown plant installed sensors that track airborne particles 24/7. If levels spike, the system shuts down the line before a batch is made. That’s not science fiction - it’s now standard for top-tier generic makers.
Regulators are catching up too. In January 2023, the FDA made nitrosamine testing mandatory for all sartan-class drugs. They’ve also upgraded their PREDICT system, which now flags 37% more risky shipments before they even reach U.S. ports. And by 2024, the FDA plans to roll out AI tools that analyze 15,000 data points per facility to predict contamination risks with 89% accuracy.
How Patients and Pharmacists Can Respond
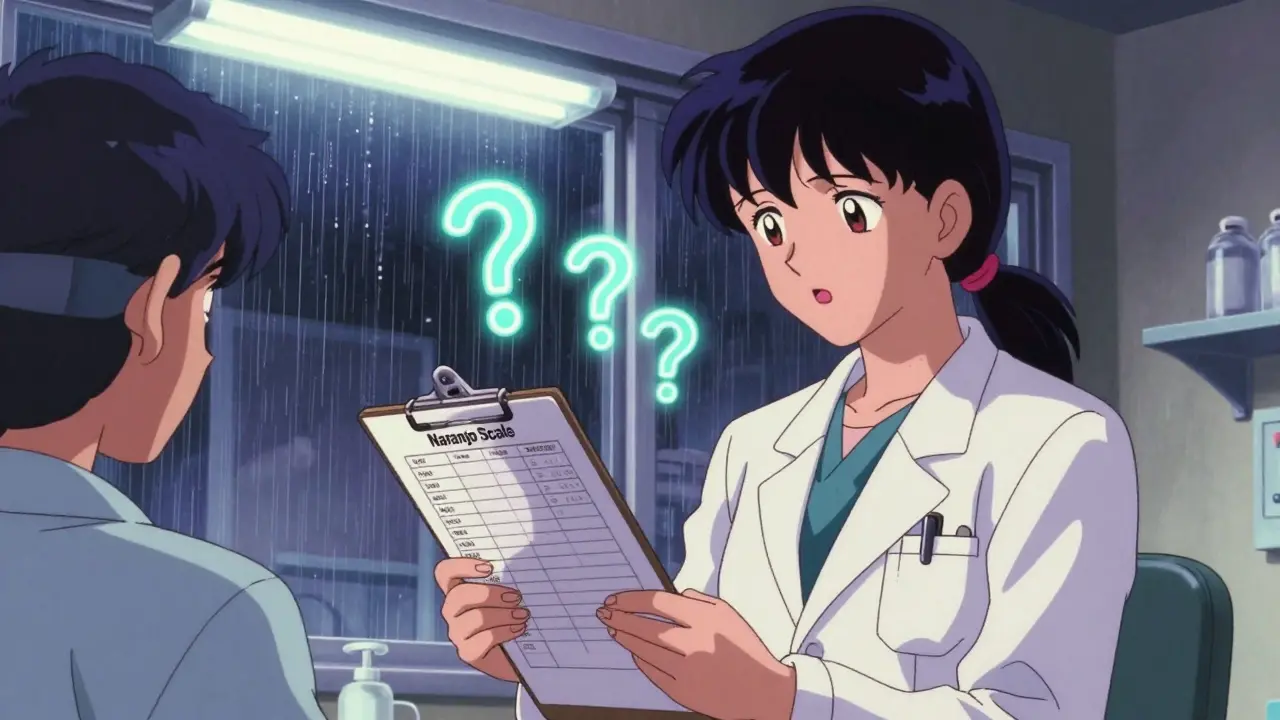
You can’t test your pills at home. But you can be alert.If your generic medication suddenly looks different - new color, odd smell, strange specks - don’t ignore it. In January 2022, a pharmacist on Reddit posted photos of blue specks in metronidazole tablets. Testing confirmed copper contamination. That drug treats bacterial infections. Copper can cause nausea, vomiting, even liver damage. The batch was recalled within days.
Pharmacists are on the front lines. A 2022 survey found 28% of hospital pharmacists had encountered suspicious generics. Of those, 14% led to patient harm. If you’re a pharmacist, report it. Use the FDA’s MedWatch system. If you’re a patient, ask your pharmacist: “Is this the same batch as before?” If the answer is vague or they can’t check, it’s worth asking for another source.
Also, know your rights. If a drug is recalled, your pharmacy must notify you. You’re entitled to a replacement or refund. Don’t just toss the bottle. Return it - and report the issue. One report won’t stop a bad batch. But 100 reports can trigger an investigation.

What You Should Expect from Your Medication
A generic drug should be identical to the brand in strength, dosage, and effect. It’s not supposed to make you sick. If you’ve had unexplained side effects - rashes, dizziness, stomach pain - that started after switching to a new generic, it’s worth investigating.Keep your medication’s lot number. It’s printed on the bottle. If there’s a recall, you can check it against the FDA’s database. You don’t need to be a scientist. Just use the lot number to search FDA recalls.
And remember: cheaper doesn’t mean worse - but it can mean less oversight. Choose pharmacies that source from reputable distributors. Chain pharmacies and hospital systems usually have tighter controls than small online sellers. If you’re buying online, stick to licensed U.S. pharmacies. Look for the VIPPS seal.
The Bottom Line
Generic drugs saved the U.S. healthcare system over $300 billion in the last decade. They’re essential. But their safety depends on constant vigilance - from manufacturers, regulators, pharmacists, and patients.The good news? The tools to prevent contamination are available. Closed systems, AI monitoring, rapid testing - they exist. The challenge is making them standard, not optional. Until then, stay informed. Speak up. And never assume a pill is safe just because it’s cheap.






Paul Ong
January 1, 2026 AT 10:11Been taking generic blood pressure meds for years and never had an issue but this post made me check my last bottle
Lot number matches the recall list from last month
Called my pharmacy they said they didn't know
Going to demand a replacement and file a report
Andy Heinlein
January 2, 2026 AT 16:38lol i just thought my stomach was upset from the new generic pills
turns out i had the same batch as the one with copper specks
took me 3 weeks to figure it out
now i always check the color and smell
also i dont buy from random online pharmacies anymore
too risky
Bobby Collins
January 3, 2026 AT 19:10theyre hiding something
the FDA is in bed with big pharma
why else would they let this keep happening
the same companies make both brand and generic
its all one big scam
they want you sick so you keep buying
the mold in hydrocortisone was intentional
to scare people into paying more for name brands
you think they care about you
they care about profit
watch your back
Layla Anna
January 4, 2026 AT 23:05thank you for writing this
i work at a small clinic and we had a patient come in with a rash after switching generics
we didnt know what to do
now i know to check the lot number and report it
also i always ask patients if they noticed any changes
little things matter
youre not alone in this
and yes i cried reading the part about pharmacists handling chemo drugs without proper hoods
that broke my heart
❤️
Heather Josey
January 6, 2026 AT 20:16This is a critical public health issue that requires immediate systemic reform
The current regulatory framework is insufficient to protect patients
Manufacturing standards must be uniformly enforced globally
Transparency in sourcing and real-time contamination monitoring should be mandatory
Patients deserve more than cost-driven compromises
Pharmacies must be held accountable for batch traceability
I urge all healthcare professionals to advocate for stricter oversight
This is not about fear
It is about responsibility
Donna Peplinskie
January 7, 2026 AT 10:12Thank you so much for sharing this… I’ve been worried about this for years
My mom switched to a generic antidepressant last year… and she started having panic attacks
We never connected it until now
She’s back on brand now
And I’ve started asking every pharmacist I meet: ‘Do you know where your generics come from?’
It’s not rude… it’s necessary
And if we all do it… they’ll have to listen
Thank you for giving me the courage to speak up
Olukayode Oguntulu
January 8, 2026 AT 23:01The ontological crisis of pharmaceutical commodification is not merely a regulatory failure
It is a symptom of late-stage capitalist epistemic collapse
The body becomes a site of neoliberal biopolitical administration
Where efficacy is reduced to pharmacokinetic equivalence
And human suffering is externalized into the Global South
The FDA’s 10 ppm standard is a neoliberal fiction
Constructed to absolve capital of bioethical responsibility
Meanwhile, the Indian pharmacist, underpaid and overworked, becomes the unwitting agent of systemic violence
And we, the consumers, are complicit in our own pharmacological alienation
What is a pill, really, but a neoliberal sacrament?
And who are we, if not the willing recipients of its poisoned grace?
jaspreet sandhu
January 9, 2026 AT 03:39Everyone is making a big deal over nothing
India makes 60 percent of the world’s generics and they are the best in the world
My cousin works in a factory in Hyderabad and they test every batch five times
The FDA is just jealous because they can’t make drugs this cheap
People in America are too lazy to take care of themselves
They think a pill will fix everything
And then they blame the medicine when they feel bad
There is no contamination problem
There is only fear and ignorance
And people who want to scare you to sell you more expensive pills
Just take your medicine and stop complaining
Alex Warden
January 10, 2026 AT 09:12Let me get this straight
China and India make our pills and now we’re scared
But we let them make our phones and TVs
And we don’t even blink
Why is this different
Because it’s medicine
And medicine is a privilege for the weak
Get real
Our country is falling apart
And you’re worried about blue specks
Fix the system
Don’t whine about pills
LIZETH DE PACHECO
January 11, 2026 AT 17:29I’m a pharmacist and I see this every day
One batch of generic metformin had a weird smell
I held it back and called the distributor
Turned out it was a batch from a plant with 12 previous violations
They pulled it
Two days later the FDA issued a recall
My point? Speak up
Don’t be shy
One voice can save someone
Lee M
January 13, 2026 AT 14:04Contamination isn’t the real problem
The real problem is that we’ve outsourced our health to a global supply chain we don’t control
And we pretend that cost savings are worth the risk
But we’re not saving money
We’re just shifting the cost onto patients
Through ER visits
Through lawsuits
Through lost work
Through death
It’s not a supply chain issue
It’s a moral failure
Kristen Russell
January 13, 2026 AT 16:45Check your lot number. Always.