Aging and Medication: How Older Adults Navigate Drug Risks and Benefits
When you get older, your body doesn’t just slow down—it starts processing drugs differently. This is aging and medication, how the body’s changing biology affects how drugs are absorbed, broken down, and cleared out. Also known as age-related pharmacokinetics, it’s why a pill that was safe at 50 can become dangerous at 75. Your liver and kidneys don’t work as fast. Fat and muscle ratios shift. And your brain becomes more sensitive to certain chemicals. These aren’t just minor changes—they turn common prescriptions into potential hazards.
That’s why polypharmacy, taking five or more medications at once. Also known as multiple drug regimens, it’s one of the biggest risks for seniors. It’s not about being on too many pills—it’s about how those pills talk to each other. Grapefruit juice can spike blood levels of statins. Antihistamines can make you dizzy and fall. Painkillers can wreck your stomach or kidneys. And many of these interactions fly under the radar because doctors focus on treating one condition at a time, not the whole person.
Then there’s age-related drug metabolism, how the body’s ability to break down and remove drugs declines with age. A drug that used to be cleared in 8 hours might now stick around for 24. That’s why lower doses often work better—and why side effects like confusion, falls, or nausea show up even with "normal" prescriptions. It’s not your fault. It’s biology. And it’s why simply following a doctor’s script isn’t always enough. You need to ask: Is this still right for me? Could a lower dose work? Are there safer alternatives?
Some of the most common problems we see in older adults? Statins causing muscle pain, blood pressure meds dropping pressure too low, sleep aids leading to daytime fog, and diabetes drugs causing dangerous lows. These aren’t rare. They happen every day. And they’re often mistaken for "just getting older." But they’re not. They’re medication side effects—and they’re often preventable.
The good news? You don’t have to accept this. There are smarter ways to manage meds as you age. You can work with your doctor to simplify your list, switch to safer drugs, or adjust doses based on how your body actually responds—not just standard guidelines. You can track what you’re taking, know which foods to avoid, and spot warning signs before they turn into emergencies.
Below, you’ll find real, practical guides on exactly how this plays out. From how grapefruit juice can interfere with heart meds to why certain painkillers are riskier after 65, these posts break down the science without the jargon. You’ll learn how to recognize dangerous interactions, understand why some drugs become unsafe with age, and find alternatives that actually work better for older bodies. This isn’t theory. It’s what people are using right now to stay healthy, safe, and in control of their own care.
Medication Dosage Adjustments for Aging Bodies and Organs: What Seniors and Caregivers Need to Know
By Lindsey Smith On 15 Nov, 2025 Comments (16)
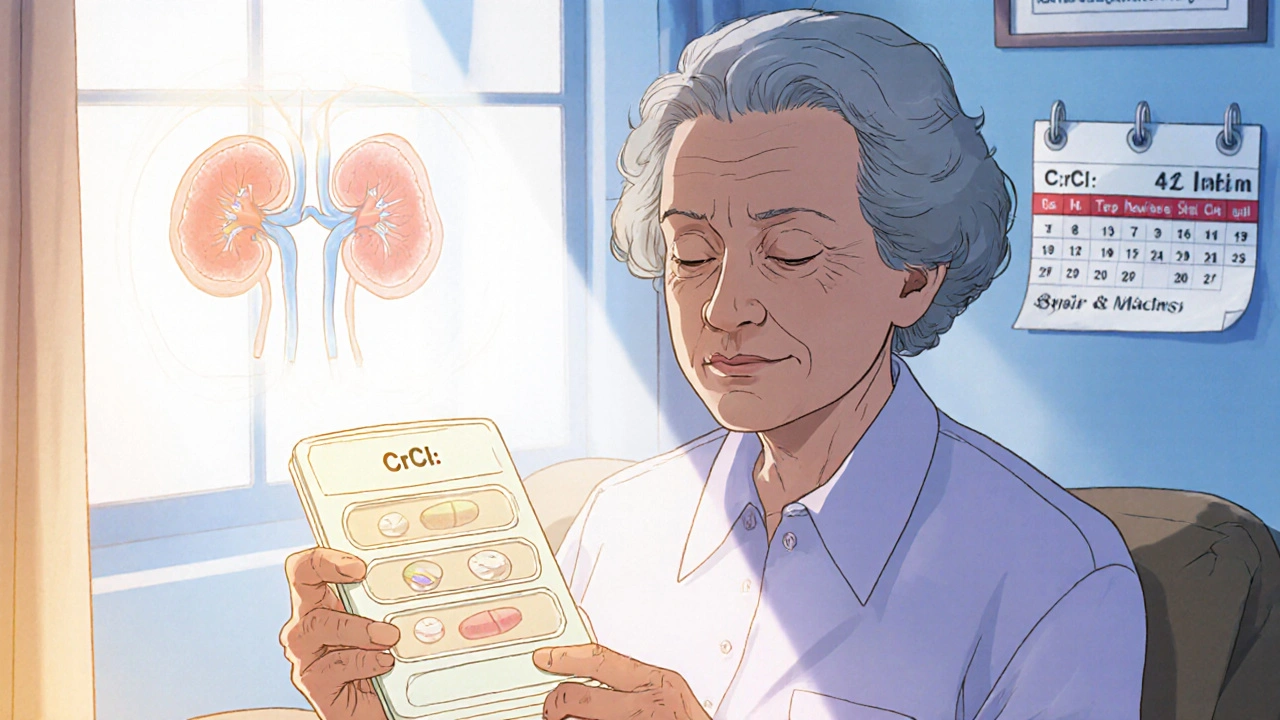
Aging changes how your body handles medication. Learn why seniors need lower doses, which drugs are risky, how kidney function affects dosing, and what you can do to avoid dangerous side effects.
View More